Managing medications for dual diagnosis – when mental health conditions and substance use disorders occur together – can be challenging. Here’s a quick guide to staying on track:
- Communicate with Your Care Team: Share your full health history and medication list with all providers to avoid risks and ensure treatments align.
- Understand Your Medications: Know why each medication is prescribed, its side effects, and how to handle missed doses.
- Coordinate Care: Ensure all providers are informed and work together to avoid conflicting treatments or harmful interactions.
- Stick to a Routine: Use tools like pill organizers or reminder apps to create a schedule that fits your daily habits.
- Monitor Side Effects: Track how medications affect you and report changes to your provider for timely adjustments.
Managing Dual Diagnosis: Addressing Co-occurring Stimulant Use Disorder
Build Clear Communication with Your Treatment Team
Managing dual diagnosis medications requires a well-coordinated effort between multiple professionals – psychiatrists, addiction specialists, primary care physicians, therapists, and pharmacists. This teamwork is essential in navigating the complexities and risks that come with dual diagnosis treatment. Each expert brings a unique perspective to ensure your care is as effective and safe as possible.
The foundation of effective medication management lies in being completely transparent about your health history. Share details about all medications, supplements, and treatments you’re using. Omitting information, even unintentionally, can lead to complications or risks that could otherwise be avoided.
Clear communication sets the stage for the detailed planning and collaboration needed for successful treatment.
Discuss Your Medication Plan Openly
It’s not enough to know what medications you’re taking – you should also understand why you’re taking them. Your healthcare team should explain the purpose behind each prescription. This understanding can keep you motivated to stick with your treatment plan, especially during moments of doubt or frustration when progress feels slow.
Ask questions like: What symptoms is this medication targeting? How long before I notice changes? What happens if I don’t see improvement? These discussions help you take an active role in your treatment rather than just following instructions passively.
Some psychiatric medications may come with side effects like drowsiness, dizziness, or changes in appetite, which could potentially trigger cravings. Bring up these concerns with your doctor so you can develop strategies to manage them. Adjustments to dosage, switching medications, or changing the timing of doses may help reduce unwanted effects.
If cost or access to a prescribed medication is an issue, don’t hesitate to speak up. Your provider may suggest more affordable alternatives or connect you with assistance programs. A treatment plan is only effective if it’s something you can follow consistently.
Once you’re clear on your medication plan, the next step is ensuring all your providers are on the same page.
Coordinate Care Between Providers
One of the biggest challenges in dual diagnosis treatment arises when healthcare providers don’t communicate with each other. For example, your psychiatrist might prescribe an antidepressant while your addiction specialist recommends a medication for cravings. Without proper coordination, these treatments could conflict or lead to unintended side effects.
To prevent this, make sure every provider involved in your care has a complete list of your current medications and knows about the other professionals on your team. This collaborative approach ensures that your treatment plan is cohesive and safe. Many people find it helpful to designate one provider, such as a primary care doctor or psychiatrist, to oversee and coordinate care across the board.
Keep a written, updated list of all your medications, including dosages and the names of prescribing doctors. Bring this list to every appointment to avoid potential oversights and to help your providers make well-informed decisions when adjusting or adding prescriptions.
You might also consider signing release forms that allow your healthcare providers to communicate directly with one another. This step can streamline the sharing of information, reducing the risk of miscommunication and ensuring everyone involved in your care has the full picture. It’s a simple yet powerful way to protect your safety and enhance the effectiveness of your treatment.
Create and Follow a Daily Medication Routine
Sticking to a consistent routine is essential when managing medications for dual diagnosis. A structured schedule not only supports your psychiatric care but also aids in addiction treatment. Missing doses or taking them irregularly can disrupt your progress and trigger symptoms, so establishing a reliable daily plan helps keep everything on track. Just as clear communication with your healthcare provider is key, so is maintaining a disciplined approach to your medication routine.
The best routine is one that fits seamlessly into your lifestyle – something you can stick with over the long haul.
Use Tools to Stay Organized
There are plenty of tools available to help you stay on top of your medication schedule. Technology can be a game-changer. For example:
- Smart blister packs come with microchips that record when a pill is removed, giving you precise tracking of your adherence.
- Electronic audiovisual reminder devices (AVRD) are pillboxes equipped with lights and alarms to alert you when it’s time for your next dose.
- AI-powered mobile apps send personalized reminders for both medication times and refills directly to your phone.
If you prefer more traditional methods, those work well too. A pill organizer with compartments for each day and time can help you set up a week’s worth of medications in advance. This visual system makes it easy to see if you’ve taken your morning or evening doses. Another simple option is carrying a pocket medicine list or wallet card for easy reference.
The key is to integrate these tools into your daily life in a way that feels natural.
Link Medication to Daily Habits
Pairing your medication with everyday activities can make sticking to your schedule feel less like a chore. By tying doses to habits you already have, you create mental cues that make it harder to forget.
For instance, morning medications can be taken with breakfast, your first cup of coffee, or during your morning bathroom routine. If you take medications that make you drowsy, it might make more sense to include them in your evening routine – right after brushing your teeth or while unwinding with your favorite TV show.
For medications that need to be taken with food, keep your pill organizer in a spot you naturally visit during meals, like next to the coffee maker or on the kitchen counter where you prepare food. The visual reminder alongside your established routine reinforces the habit.
If your medication needs to be spaced throughout the day, tie doses to consistent activities. For example, take your afternoon medication when you check emails after lunch or place your evening dose next to your phone charger so you see it when plugging in your device before bed.
By linking your medication to regular habits, you eliminate the need for extra effort and make adherence easier.
What to Do If You Miss a Dose
Even with the best routine, missed doses can happen. Knowing how to handle these situations calmly and effectively is important.
For most medications, if you remember within a few hours, take the missed dose right away. But if it’s close to the time of your next dose, skip the missed one and stick to your regular schedule. Never double up on doses – doing so can lead to harmful side effects or interactions.
For psychiatric medications, missed doses may require special attention. Some antidepressants or mood stabilizers can cause withdrawal-like symptoms if skipped, while others might lead to a return of symptoms. If you miss a dose, reach out to your prescribing doctor for advice instead of guessing.
Medications for addiction treatment, such as naltrexone or buprenorphine, have their own specific protocols for missed doses. Your addiction specialist should provide clear instructions for these scenarios during your treatment planning.
It’s also helpful to keep a record of missed doses in a journal or app. This allows you to discuss any patterns with your treatment team so they can help you adjust your routine if needed.
If missed doses become frequent, it’s a sign to reevaluate your current system. Instead of simply trying harder, work with your healthcare provider to identify barriers and find strategies that better fit your lifestyle.
Monitor and Report Side Effects and Changes
Alongside keeping up with your medication routine and communication with your healthcare team, it’s equally important to stay mindful of how your body responds to treatment. When managing both mental health conditions and addiction recovery, a dual diagnosis can sometimes bring about unique side effects. These effects might influence your daily life, impact your recovery, or signal the need for changes in your treatment plan.
Paying attention to both physical and mental changes allows your healthcare provider to make better decisions about your care. The goal here isn’t to stress over every small change but to recognize what’s typical for you and what might need further attention. This kind of awareness helps you and your healthcare team better understand common side effects.
Understand Common Side Effects
Medications prescribed for dual diagnoses often come with side effects such as nausea, headaches, drowsiness, or appetite changes. Fortunately, many of these subside within 4–6 weeks.
For example, mood stabilizers like lithium or valproate can lead to weight gain, tremors, or increased thirst and urination. Lithium, in particular, requires regular bloodwork to monitor its impact on kidney and thyroid function.
Anti-anxiety medications, including lorazepam (Ativan) or clonazepam (Klonopin), might cause drowsiness, dizziness, or memory issues. These medications can carry a risk of dependency, which makes careful monitoring especially important in the context of addiction recovery.
Similarly, medications used for addiction treatment come with their own side effects. For instance, naltrexone might lead to nausea, fatigue, or headaches, while buprenorphine can cause constipation, sweating, or sleep disturbances.
If side effects interfere with your ability to work, maintain relationships, or manage daily tasks, reach out to your healthcare provider. They may adjust your dosage, switch medications, or suggest ways to manage these symptoms.
Know When to Seek Medical Attention
While most side effects are manageable, certain symptoms require immediate medical attention.
Seek emergency care if you experience signs of anaphylaxis, severe heart issues, or neurological changes. Symptoms like difficulty breathing, swelling in the tongue or throat, trouble swallowing, or severe hives point to anaphylaxis – a potentially life-threatening reaction that demands urgent treatment.
“Adverse drug reactions are the fourth leading cause of death in the United States, resulting in more than 106,000 deaths each year”.
For less urgent but concerning symptoms – such as persistent vomiting that prevents you from taking medication, drastic mood changes (including thoughts of self-harm), or severe, unrelenting dizziness – contact your healthcare provider within 24 hours.
For those with a dual diagnosis, it’s important to stay extra cautious about symptoms that could indicate medication interactions or complications from a complex treatment plan. If you’re unsure whether a symptom needs urgent attention, don’t hesitate to call your healthcare provider or a nurse advice hotline for guidance.
It’s worth noting that drug allergies account for less than 10% of all adverse drug reactions, while side effects make up over 90%. This means most reactions you encounter will likely be manageable side effects, though it’s always wise to remain cautious.
Track Changes Over Time
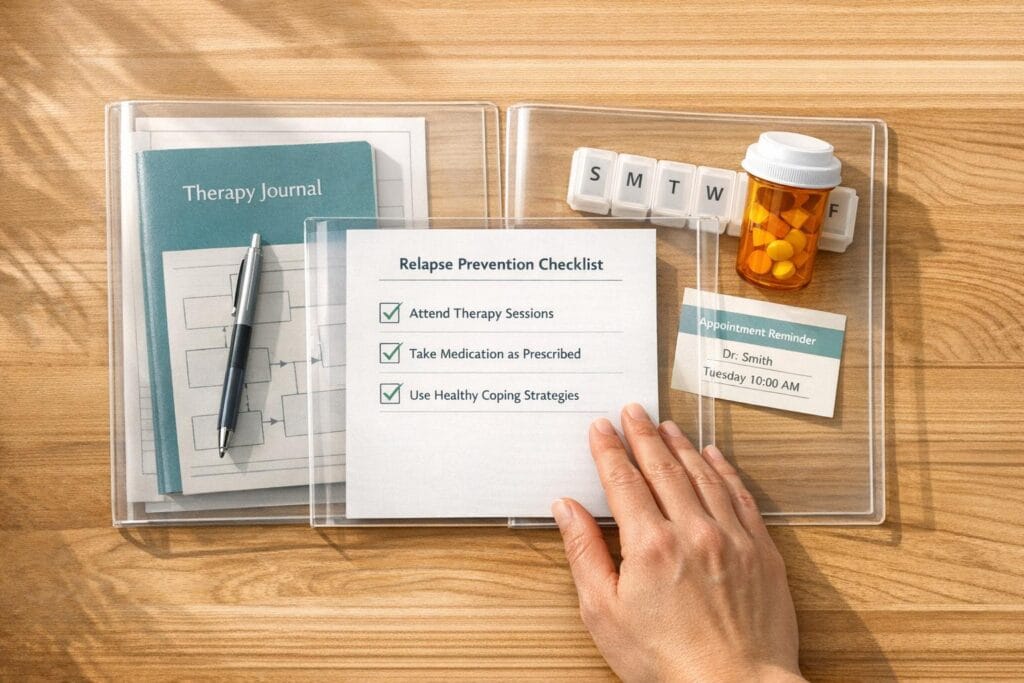
Keeping a detailed record of your experiences with medication can make a big difference in helping you and your healthcare team identify patterns and make informed decisions. A medication journal is especially helpful when juggling multiple medications and conditions.
Document each dose, any side effects, and your overall well-being. Include both physical symptoms (like headaches, nausea, or fatigue) and emotional shifts (such as mood changes, anxiety levels, or sleep quality). Rate the severity of symptoms on a scale to track changes more easily.
It’s also useful to track your recovery progress alongside medication effects. Note cravings, energy levels, focus, or how well you’re managing daily responsibilities. This kind of information helps your treatment team evaluate whether your medications are effectively supporting your recovery goals.
Whether you use a notebook or an app, logging information like dose times, side effects, mood changes, and missed doses can reveal patterns over time. For instance, you might notice that certain side effects worsen during stressful periods or that taking medication at a different time of day improves its effectiveness.
Your medication journal isn’t just a record – it’s a tool for advocating for your care. By documenting your experiences, you help ensure that your treatment plan evolves to meet your needs as you progress in your recovery.
For more resources on managing dual diagnosis and recovery, visit Sober Living Centers.
sbb-itb-17645e5
Understand Drug Interactions and Contraindications
When managing medications for dual diagnoses, it’s crucial to keep an eye on how different substances might affect their effectiveness or lead to unwanted side effects.
Be Cautious of Harmful Interactions
Certain substances can interfere with your medication, reducing its effectiveness or even causing harmful reactions. For example, alcohol, over-the-counter medications, and herbal supplements can sometimes disrupt your treatment plan. Even seemingly minor interactions can lead to unexpected complications. Always consult your healthcare provider before adding anything new to your routine, no matter how harmless it may seem.
Share All Substance Use Honestly
Make sure to share a complete list of everything you’re taking with your provider. This includes prescription medications, over-the-counter drugs, vitamins, herbal remedies, and recreational substances. Be specific about how often you use them and in what amounts. This transparency helps your provider adjust your treatment to reduce risks and improve outcomes. Plus, your disclosures are protected by confidentiality laws, ensuring your privacy.
Being mindful of these interactions is an essential part of a well-rounded treatment plan for dual diagnoses.
Combine Medication Management with Therapy and Support
Once you’ve established good communication and daily routines, adding therapy and support can take your medication management to the next level. Medications work best when paired with therapy, lifestyle adjustments, and a supportive community – especially for those navigating dual diagnosis recovery.
Pair Medication with Therapy
Therapy combined with medication creates a more balanced and effective treatment plan. Approaches like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and motivational interviewing can significantly improve medication adherence in dual diagnosis treatment.
- CBT helps you uncover and address negative thought patterns that may interfere with sticking to your medication plan.
- DBT focuses on emotional regulation and mindfulness, which can make it easier to handle side effects and cravings.
- Motivational interviewing encourages open, judgment-free conversations about your doubts or hesitations around medication, helping you clarify personal reasons to stay committed to your treatment.
Adopt Healthy Lifestyle Practices
Your daily habits can influence how well your medications work. Paying attention to nutrition, exercise, sleep, and stress management can maximize benefits and minimize side effects.
- Eating balanced meals keeps your blood sugar steady, which supports mood regulation and curbs cravings.
- A simple 30-minute walk each day can amplify the effects of antidepressants and ease withdrawal symptoms.
- Sticking to a consistent sleep schedule helps your body adapt to medication routines.
- Stress management techniques, like deep breathing or meditation, can reduce reliance on anxiety medications taken as needed.
Use Support Groups and Community Resources
Support from peers and family can offer accountability, guidance, and encouragement throughout your recovery journey. Groups like Dual Recovery Anonymous are tailored to individuals managing both mental health challenges and substance use disorders.
Involving family members in your treatment plan can also make a big difference. They can offer reminders, help monitor side effects, and provide emotional support during tough moments. Including trusted loved ones in discussions with your healthcare providers can strengthen your overall plan.
Organizations like Sober Living Centers offer valuable resources on addiction recovery and treatment, including how medications fit into larger recovery efforts. Their educational materials can help you better understand the connection between mental health and substance use, empowering you to take an active role in your care.
Local community mental health centers often host medication management support groups. These groups provide a space to share experiences, learn practical tips, and stay motivated to stick with your treatment plan.
Conclusion
The strategies discussed above offer a practical framework for managing medications in dual diagnosis treatment, helping to support both recovery and overall well-being.
Clear communication ensures that your treatment plan remains aligned and minimizes the risk of harmful interactions. By building consistent daily routines, medication management becomes a seamless part of your life, with tools and plans in place to handle missed doses and avoid disruptions.
Staying proactive by monitoring and reporting side effects allows you to take an active role in your care, enabling timely adjustments to medications when necessary. Being informed about drug interactions and transparent about all substance use further safeguards your health and enhances the effectiveness of your treatment.
Combining medication with therapy and healthy lifestyle habits creates a comprehensive approach to recovery. Techniques like CBT or DBT, along with strong community support, address both the physical and psychological challenges of dual diagnosis.
For additional guidance, Sober Living Centers offers educational resources on addiction recovery and treatment options. These materials can help individuals and families understand how medications fit into a broader recovery plan, empowering them to make informed decisions and stay connected with their care teams.
Ultimately, effective medication management relies on collaboration between you, your healthcare providers, and your support network. With the right strategies and resources, you can navigate the complexities of dual diagnosis treatment and work toward lasting recovery.
FAQs
How can I make sure all my healthcare providers work together when managing my dual diagnosis medications?
To keep your healthcare team on the same page, always bring a detailed list of your medications to every appointment. This simple step minimizes the chance of mistakes and ensures your medications are reviewed and updated correctly. Make sure to inform all your providers about any changes in your treatment plan or new prescriptions.
If available, shared electronic health records can be a great tool to enhance communication among your providers. You might also consider scheduling regular check-ins or team meetings with your care team to ensure everyone is aligned on your treatment plan. These efforts can make managing medications for dual diagnoses safer and more efficient.
How can I effectively manage medication side effects during dual diagnosis treatment?
Managing medication side effects in dual diagnosis treatment means staying proactive and engaged in your care. One of the most important steps is keeping an open line of communication with your healthcare provider. If you notice any side effects, bring them up right away. Your doctor can adjust your dosage or explore other medication options to help ease any discomfort.
It’s also crucial to schedule regular check-ins with your provider. These appointments allow your doctor to track your progress and address any emerging concerns early on. If you’re on multiple medications, careful coordination of your treatment plan is key to avoiding harmful drug interactions. By staying informed about your medications and closely following your provider’s recommendations, you can better manage side effects and stay focused on improving your overall well-being.
How can therapy and lifestyle changes help improve my medication plan for dual diagnosis?
Therapies like cognitive-behavioral therapy (CBT) are designed to help you recognize and tackle negative thought patterns and behaviors that might be getting in the way of your recovery. By addressing these challenges, it becomes easier to stay consistent with your medication plan, ultimately improving your overall progress.
On top of that, embracing healthier lifestyle choices – such as staying active, eating nutritious meals, managing stress effectively, and steering clear of harmful substances – can boost both your mental and physical health. Together, these habits complement your medications, enhancing their effectiveness and supporting long-term recovery.