When you drink alcohol, it doesn’t take long to affect your body. Within minutes, it enters your bloodstream, influencing your brain, reflexes, and overall coordination. Short-term risks include:
- Dehydration: Alcohol is a diuretic, leading to fluid and electrolyte loss, causing thirst, fatigue, and headaches.
- Nausea and Vomiting: Alcohol irritates your stomach lining and produces toxic byproducts, triggering nausea and potential vomiting.
- Slowed Reflexes and Loss of Coordination: Alcohol disrupts brain-body communication, impairing motor skills and balance.
- Slurred Speech: Alcohol affects muscle coordination, making clear speech difficult.
- Blurred Vision: Drinking impacts eye-brain coordination, causing vision problems like double vision or difficulty focusing.
- Hangover Symptoms: Dehydration, fatigue, headaches, and nausea often follow excessive drinking.
- Flushed Skin and Redness: A reaction to alcohol’s toxic byproducts, common in certain genetic groups.
- Increased Heart Rate and Blood Pressure: Alcohol can strain your cardiovascular system, with effects lasting up to 24 hours.
- Frequent Urination: Alcohol suppresses a hormone that helps retain water, leading to excessive bathroom trips.
These effects vary based on factors like your weight, age, and genetic makeup. Drinking responsibly and staying hydrated can help reduce risks. If you notice severe symptoms like irregular breathing, unresponsiveness, or prolonged vomiting, seek medical attention immediately.
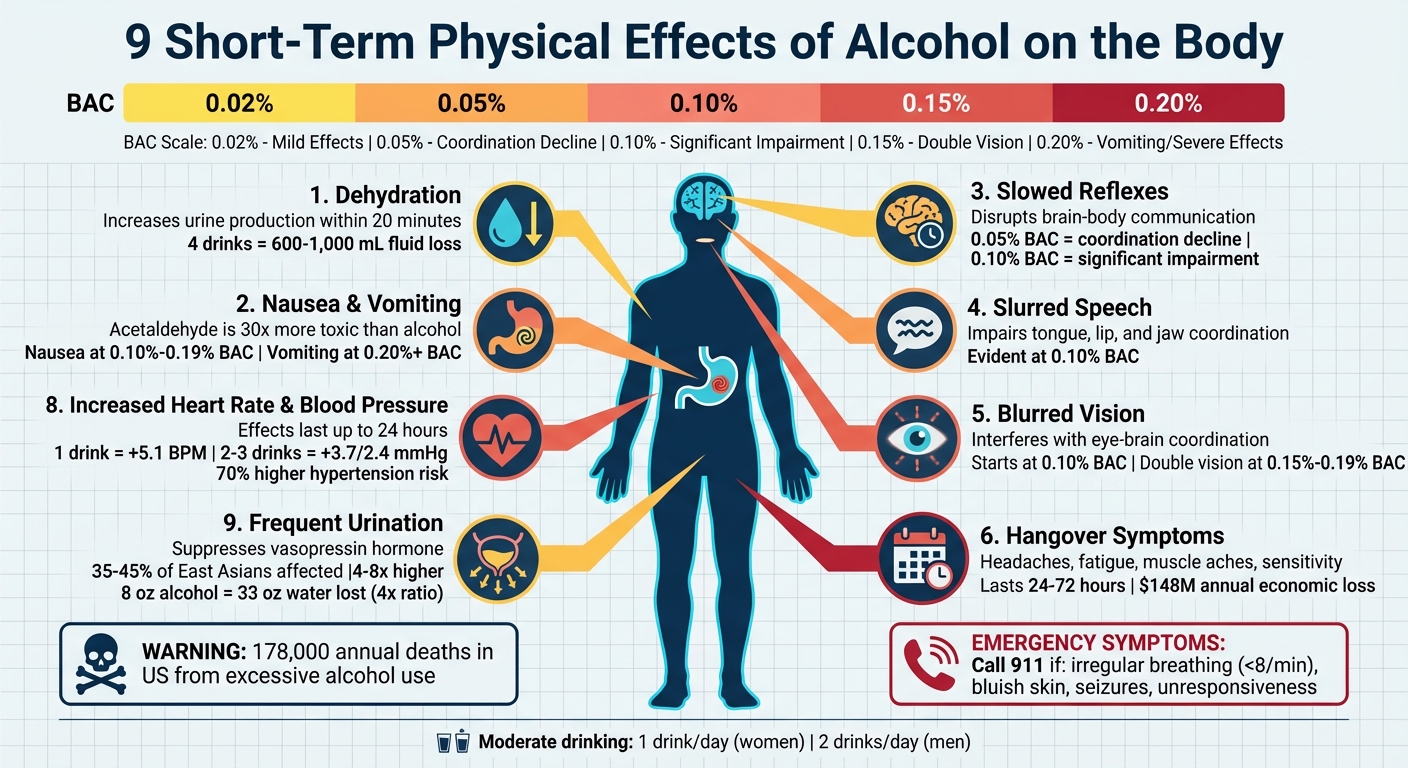
9 Short-Term Physical Effects of Alcohol on the Body
What Alcohol Really Does to Your Body: Short & Long-Term Risks Explained
sbb-itb-17645e5
1. Dehydration
One of the most immediate effects of alcohol is dehydration. Alcohol acts as a diuretic, meaning it increases urine production and causes your body to lose fluids quickly. This happens because alcohol suppresses vasopressin, a hormone that tells your kidneys to retain water. Without it, your kidneys let water pass right through instead of reabsorbing it.
The dehydration process kicks in fast. Within 20 minutes of drinking, alcohol ramps up urine production. Drinking just four alcoholic beverages can lead to the loss of 600 to 1,000 mL of fluid in just a few hours. This rapid fluid loss often results in thirst, fatigue, and headaches – all hallmarks of a hangover.
But there’s more to it than just frequent trips to the bathroom. Alcohol also causes vasodilation, which is the widening of blood vessels. This raises your skin temperature and triggers sweating, leading to even more fluid loss. On top of that, essential electrolytes like sodium, potassium, and magnesium are flushed out, disrupting your body’s fluid balance. Hyponatremia, or low sodium levels, is a common issue for people who drink regularly.
To combat dehydration, try drinking a 16-oz glass of water with each alcoholic beverage. Stick to no more than one drink per hour to give your liver enough time to process the alcohol. For better hydration, consider electrolyte-rich options like coconut water or sports drinks. These help replenish sodium and potassium more effectively than plain water.
2. Nausea and Vomiting
Alcohol doesn’t just dehydrate you – it also wreaks havoc on your stomach and digestive system. It irritates the stomach lining, ramps up acid production, and produces acetaldehyde during metabolism. This toxic byproduct, which is estimated to be 30 times more harmful than alcohol itself, irritates the gastrointestinal tract and triggers the brain’s vomiting center.
How bad the nausea gets often depends on how much you drink. For example, nausea might kick in when your blood alcohol concentration (BAC) hits 0.10%–0.19%. Once your BAC climbs above 0.20%, vomiting becomes more likely. Dr. Robert Swift explains:
Acetaldehyde is a highly reactive toxin that binds to proteins and other biologically important compounds. At higher concentrations, it causes toxic effects, such as a rapid pulse, sweating, skin flushing, nausea, and vomiting.
Drinking heavily also slows down how quickly your stomach empties, leaving it exposed to irritants for longer. This effect is even worse with darker spirits, which contain more congeners – compounds that can make nausea and other symptoms more intense compared to clear spirits.
If you’re feeling queasy, give yourself at least 30 minutes before consuming any more alcohol. Start with small sips of water or weak tea – about 1–2 ounces at a time. Steer clear of carbonated drinks and avoid the “hair of the dog” approach, as neither will actually help you recover. Eating a meal rich in protein and healthy fats before drinking can also help by slowing alcohol absorption and reducing acetaldehyde buildup.
Keep in mind that nausea and vomiting can make dehydration worse, amplifying your discomfort. If vomiting lasts more than 24 hours, you notice blood in your vomit, or you experience severe dehydration symptoms like dark urine or dizziness, seek medical attention immediately. For unconscious individuals who vomit, there’s a serious danger of aspirating vomit into the lungs, which can lead to life-threatening complications.
3. Slowed Reflexes and Loss of Coordination
Alcohol, as a central nervous system depressant, starts to interfere with brain function and motor skills almost immediately after consumption. It disrupts the communication between your brain and body, leading to noticeable physical impairments within minutes.
The cerebellum, the part of the brain responsible for movement, balance, and coordination, is particularly affected. Alcohol’s impact on sodium-potassium pumps in the cerebellum leads to a condition called ataxia. This results in jerky movements, difficulty maintaining balance, and an unsteady gait. These effects not only make movements awkward but also contribute to broader motor control issues. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) explains:
Alcohol interferes with the brain’s communication pathways and can affect the way the brain looks and works. These disruptions can change mood and behavior and make it harder to think clearly and move with coordination.
Alcohol also affects the inner ear, which plays a key role in balance. By altering the viscosity of inner ear fluids, it causes exaggerated balance signals that lead to vertigo, often referred to as “the spins”. At higher levels of intoxication, alcohol can even suppress automatic protective reflexes, such as the gag reflex, increasing the risk of choking on vomit.
The degree of impairment directly correlates with blood alcohol concentration (BAC). For instance:
- At 0.05% BAC, coordination begins to deteriorate.
- At 0.10%, motor skills and reflexes are significantly impaired.
- At 0.15%, critical abilities like visual and auditory processing, as well as vehicle control, are severely compromised.
Studies show that the risk of car accidents rises sharply with even small increases in BAC. These motor impairments are a major factor in the immediate dangers associated with alcohol consumption. For those struggling with long-term dependency, finding a dedicated addiction and recovery resource can be a vital step toward safety.
If you’ve been drinking, it’s essential to avoid tasks that require quick reflexes or alertness, such as driving or operating machinery. Additionally, if someone nearby is heavily intoxicated and unconscious, roll them onto their side with one ear toward the ground to reduce the risk of choking, as their gag reflex might not function properly.
4. Slurred Speech
Alcohol doesn’t just affect coordination and reflexes – it also disrupts verbal communication.
Slurred speech is one of the most noticeable signs that alcohol is impairing brain function. As a central nervous system depressant, alcohol increases GABA (gamma-aminobutyric acid) activity while reducing glutamate. This chemical imbalance impacts the fine motor control needed for clear speech, including the coordination of the tongue, lips, and jaw.
Dr. Akhil Anand, an addiction psychiatrist at Cleveland Clinic, highlights:
When alcohol overloads the liver’s enzymes, muscle coordination deteriorates, resulting in slurred speech.
Typically evident at a blood alcohol concentration (BAC) of around 0.10%, slurred speech – technically referred to as dysarthria – occurs because the brain struggles to manage the precise motor skills required for speaking clearly.
If you notice someone’s speech becoming slurred, it’s a strong indicator their BAC has likely surpassed safe levels. At this point, drinking should stop immediately. While slurred speech usually resolves as the body metabolizes alcohol, it’s a warning sign of deeper impairments that can endanger safety. Additionally, if slurred speech persists while sober, it could point to long-term brain damage from chronic alcohol use, making a medical evaluation essential.
5. Blurred Vision
Alcohol doesn’t just affect your ability to move or speak – it also impacts your vision. This happens because alcohol interferes with the coordination between your eyes and brain, leading to blurred vision.
Here’s how it works: Alcohol acts as a depressant on the central nervous system, slowing down visual processing and impairing eye muscle control. Normally, your brain adjusts for small imbalances in eye muscle coordination to keep your vision clear. But alcohol relaxes this control, making those imbalances more noticeable – and your vision less sharp.
Blurred vision can start at a blood alcohol concentration (BAC) of 0.10%, but even a BAC as low as 0.02% may cause subtle tracking issues. At higher levels, between 0.15% and 0.19% BAC, double vision and pronounced blurriness often occur. Alcohol can also cause horizontal gaze nystagmus, a condition where your eyes jerk involuntarily, making smooth tracking nearly impossible. Night vision takes a hit too, with halos or starbursts appearing around lights.
If you notice any visual difficulties while drinking, avoid driving or handling machinery until the alcohol has left your system. Blurred vision typically clears up as your body processes the alcohol. However, if the problem persists after you’ve sobered up, it’s a good idea to see an ophthalmologist, as it could point to another underlying issue.
6. Hangover Symptoms
A hangover is your body’s way of bouncing back after alcohol consumption. Symptoms usually show up a few hours after drinking, often hitting the hardest the next morning when the alcohol has been fully processed by your body.
The rapid fluid loss that alcohol triggers sets the stage for hangover symptoms. These can include headaches, nausea, thirst, muscle aches, fatigue, dizziness, sensitivity to light and sound, increased heart rate, excessive sweating, red eyes, and tremors. Besides being unpleasant, hangovers can impact productivity and are linked to economic losses estimated at around $148 million annually.
Most hangovers fade within 24 hours, but in some cases, symptoms can linger for up to 72 hours. As the National Institute on Alcohol Abuse and Alcoholism puts it:
There is no cure for a hangover other than time.
Your body needs time to flush out toxins, rehydrate, and get your brain back to normal functioning – there’s no shortcut to speed this up.
That said, you can take steps to feel a bit better while you wait it out. Stay hydrated with water or drinks rich in electrolytes and nibble on bland carbs like toast to stabilize your blood sugar. Over-the-counter pain relievers like ibuprofen or aspirin can help with aches, but steer clear of acetaminophen (Tylenol), as it can harm your liver if alcohol is still in your system. And forget the “hair of the dog” trick – drinking more alcohol just delays recovery and adds to the strain on your body. Focus instead on hydration and simple remedies to support your body as it recovers.
7. Flushed Skin and Facial Redness
Flushed skin after drinking isn’t just a surface-level reaction – it’s your body signaling a toxic buildup of acetaldehyde, a harmful byproduct of alcohol metabolism. Normally, your liver processes alcohol into acetaldehyde, which is then broken down by an enzyme called ALDH2. But if ALDH2 is deficient or doesn’t function properly, acetaldehyde accumulates, causing blood vessels to dilate and more blood to rush to the skin’s surface. This is what causes the redness and warmth often associated with drinking.
Dr. Melissa Piliang, a dermatologist at Cleveland Clinic, explains it this way:
Alcohol is toxic to cells, and when it gets into the cells of your blood vessels, it makes them dilate. This reddens your skin and can make you feel warm.
This reaction is especially common in people of East Asian descent. Roughly 35% to 45% of individuals from Chinese, Japanese, and Korean backgrounds carry a genetic variation that leads to what’s often called “Asian flush”. But genetics aren’t the sole factor. For those with rosacea, a condition that makes facial blood vessels overly sensitive, alcohol can trigger a similar flushing response. Certain medications, like disulfiram (used for alcohol use disorder) and some drugs for diabetes or infections, can also interfere with acetaldehyde breakdown, leading to redness.
Here’s why this matters: facial flushing isn’t just an inconvenience – it’s a warning sign from your body. Acetaldehyde is classified as a carcinogen, and individuals with ALDH2 deficiency who continue drinking face a four to eight times greater risk of developing esophageal cancer compared to those without the deficiency. The National Institute on Alcohol Abuse and Alcoholism clarifies:
The alcohol flush reaction is a type of alcohol intolerance – not an ‘alcohol allergy’ – and is a condition predominantly due to inherited variations in genes of certain enzymes.
It’s also important to avoid antihistamines as a quick fix. While they might reduce the redness, they don’t address the underlying acetaldehyde toxicity and could encourage further drinking. If you experience flushing, it’s a clear signal from your body to stop drinking and hydrate instead. For individuals with this enzyme deficiency, the safest choice is to avoid alcohol entirely or set strict limits on consumption.
Up next, let’s look at how alcohol impacts your cardiovascular system.
8. Increased Heart Rate and Blood Pressure
Drinking alcohol can push your heart into overdrive, with its effects lasting up to 24 hours after consumption. Even a small amount – less than 14 grams, or about one standard drink – can elevate your heart rate by an average of 5.1 beats per minute within six hours. With larger quantities, this increased heart rate can persist throughout the day, forcing your cardiovascular system to work harder than usual.
Alcohol also impacts blood pressure in a two-phase process. Initially, it relaxes blood vessels, causing a temporary drop in blood pressure for up to 12 hours. However, after this period, blood pressure rebounds, rising significantly around 13 hours post-drinking. Consuming more than 30 grams of alcohol (roughly two to three drinks) can push systolic pressure up by 3.7 mmHg and diastolic pressure by 2.4 mmHg during this rebound phase. Dr. Leslie Cho of Cleveland Clinic emphasizes:
The myth that wine is beneficial for heart health is no longer true.
Binge drinking – defined as four or more drinks for women or five or more for men within two hours – puts even more strain on the heart. This can lead to tachycardia, where your heart rate exceeds 100 beats per minute, potentially triggering dangerous arrhythmias like atrial fibrillation. This condition, often referred to as “Holiday Heart Syndrome”, can occur even in people who drink infrequently. The risks escalate if you have pre-existing health issues or combine alcohol with stimulants like cocaine, which can cause sudden and life-threatening spikes in heart rate and blood pressure.
The statistics are alarming: regular heavy drinkers are 70% more likely to develop hypertension compared to those who abstain from alcohol. To protect your heart, pace your drinking, stay hydrated, and if you have any cardiovascular concerns, it’s best to limit or avoid alcohol altogether.
Next, we’ll look at how alcohol affects urinary frequency.
9. Frequent Urination
When you drink alcohol, it works as a diuretic, speeding up water loss in your body. This happens because alcohol suppresses vasopressin – a hormone that tells your kidneys to hold onto water. Without it, your body signals you to urinate more frequently, often leading to repeated trips to the bathroom during the night [56,57].
The problem doesn’t stop there. The amount of water lost can be staggering. For every 8 ounces of alcohol you consume, your body might expel up to 33 ounces of water – nearly four times the liquid you drank. If you consume 10 to 12 units (equivalent to about five or six standard drinks), alcohol levels can become toxic, forcing your body to work overtime to flush it out.
Frequent urination also drains your body of key minerals like sodium and potassium. This, combined with fluid loss, contributes to dehydration and those dreaded morning-after headaches. The NHS explains:
Your body attempts to quickly pass out the alcohol in your urine. This will leave you feeling badly dehydrated in the morning, which may cause a severe headache.
Interrupted sleep is another downside. Waking up repeatedly to use the bathroom disrupts REM sleep, the crucial stage your body needs for proper recovery [56,57]. Some alcoholic drinks, like carbonated beers, acidic wines, or sugary cocktails, can make things worse by irritating your bladder lining, increasing the need to urinate.
To reduce these effects, try alternating each alcoholic drink with a full glass of water. This helps replenish lost fluids and slows your drinking pace [56,58]. Avoid drinking alcohol within two to three hours of bedtime to limit nighttime bathroom trips. Opt for less irritating options like diluted clear spirits instead of acidic or carbonated drinks. Eating a balanced meal before drinking can also help slow alcohol absorption, giving your body more time to process it.
Conclusion
Alcohol’s short-term physical effects can escalate rapidly, ranging from dehydration and nausea to slowed reflexes and an increased heart rate. In the United States, excessive alcohol use claims approximately 178,000 lives annually, with about one-third of these deaths stemming from acute injuries sustained while intoxicated. Understanding how alcohol impacts the body in the hours following consumption is crucial for making safer choices and identifying when someone may need emergency medical care. Recognizing these risks can help save lives when dangerous symptoms arise.
Even after drinking stops, alcohol’s dangers remain. Blood alcohol concentration (BAC) can continue to rise, even if someone has passed out. This makes it unsafe to assume an unconscious person will simply “sleep it off.” As BAC increases, individuals may face severe complications like hypothermia, memory loss, or effects resembling anesthesia – any of which could become life-threatening. Critical signs of alcohol poisoning include irregular breathing (fewer than 8 breaths per minute), bluish skin, seizures, or unresponsiveness. If you notice these symptoms, call 911 immediately and place the person on their side to reduce the risk of choking.
To minimize risks, follow moderate drinking guidelines: no more than one drink per day for women and no more than two drinks per day for men.
FAQs
How long do alcohol’s short-term effects last?
The immediate effects of alcohol typically last a few hours, though this depends on how fast your body breaks it down. On average, the body processes alcohol at a rate of about one standard drink per hour. However, this rate can differ based on factors such as your age, weight, and liver function.
Why do some people flush or turn red after drinking?
Flushing or redness after drinking is commonly linked to an inherited enzyme deficiency or conditions such as rosacea. This response, called alcohol flush reaction, happens when the body has difficulty breaking down alcohol properly. As a result, noticeable redness, particularly on the face, can occur.
When should I go to the ER for alcohol symptoms?
If someone displays signs of alcohol poisoning, such as trouble breathing (fewer than eight breaths per minute or irregular breathing), losing consciousness, seizures, bluish or pale skin, or being unresponsive, seek emergency medical help right away. These are critical symptoms that demand immediate attention from healthcare professionals.