Dual diagnosis – when someone has both a mental health condition and a substance use disorder – requires targeted care to prevent relapse. Without proper treatment, one condition worsens the other, creating a cycle that’s hard to break. Therapy and medication are the two main strategies for relapse prevention, each addressing different aspects of recovery.
- Therapy: Focuses on managing triggers, emotions, and behaviors. Methods like CBT, DBT, and Motivational Interviewing provide tools to handle cravings and prevent setbacks.
- Medication: Stabilizes brain chemistry, reduces cravings, and treats underlying mental health issues. Examples include methadone for opioid addiction or SSRIs for depression.
Key stats:
- 50% relapse within 12 weeks after inpatient care.
- Only 8% of individuals with dual diagnoses receive treatment for both conditions.
- Therapy can lower relapse rates by up to 60%, while medications like naltrexone can block substance effects and ease cravings.
Best approach: Combining therapy and medication offers the most effective path to recovery, addressing both the psychological and biological factors of dual diagnosis. Integrated treatment plans tailored to individual needs are critical for long-term success.
How Is Relapse Prevention Different For Dual Diagnosis?
sbb-itb-17645e5
What Is Dual Diagnosis and Why Relapse Prevention Is Important
Dual diagnosis refers to the coexistence of mental health disorders and substance use disorders, where each condition exacerbates the other. When mental health issues remain untreated, individuals may turn to substances like drugs or alcohol as a way to cope. Unfortunately, substance use can alter brain chemistry, worsening psychiatric symptoms in the process.
This creates a vicious cycle. Substance use often masks underlying mental health issues, making it harder to diagnose and treat them accurately. For instance, cocaine use can temporarily hide symptoms of depression, making it challenging to identify the root mental health condition.
Relapse prevention becomes significantly more complex when dual diagnosis is involved. In typical addiction treatment, symptoms such as anxiety or depression often improve after detox. However, for individuals with dual diagnosis, stopping substance use can bring untreated mental health disorders to the surface. As AddictionCenter explains:
“Because many people who have a dual diagnosis often start misusing drugs to self-medicate their mental health disorder, so when they go into sobriety, their mental health disorder is exposed, uninhibited, and untreated, with symptoms in full effect”.
This sudden exposure of untreated symptoms can create an immediate risk of relapse.
The statistics paint a stark picture. Around 50% of individuals with a substance use disorder will also experience a mental health disorder at some point in their lives, and vice versa. Yet, treatment remains insufficient – only 8% of the 9.2 million adults with co-occurring disorders in 2018 received care for both conditions. Without integrated treatment, nearly half of patients relapse within 12 weeks after completing inpatient care.
Specialized relapse prevention strategies are critical because standard addiction treatments often fail to address the psychiatric factors that act as both triggers and consequences of relapse. For example, individuals with bipolar disorder have a 61% lifetime prevalence of co-occurring substance use disorders, while those with schizophrenia face a 47% rate. These numbers highlight the importance of treatment plans that monitor overlapping warning signs – like reduced sleep, which could signal both a manic episode and heightened substance cravings. Without a coordinated approach that tackles both conditions simultaneously, patients risk becoming trapped in a cycle of relapse and crisis. In the next section, we’ll look at how therapy and medication can help break this cycle and promote long-term recovery.
Therapy Methods for Preventing Relapse
Therapy provides essential tools to help dual diagnosis patients prevent relapse by equipping them with strategies to handle triggers and cravings. In fact, studies indicate that Cognitive Behavioral Therapy (CBT) can lower relapse rates by up to 60%, making it a key approach in treatment plans.
Three therapy methods – CBT, Dialectical Behavior Therapy (DBT), and Motivational Interviewing – focus on different aspects of the relapse process. CBT targets harmful thought patterns that lead to substance use. DBT emphasizes emotional regulation to manage intense feelings, while Motivational Interviewing helps patients build the commitment they need to maintain recovery. Kathleen M. Carroll, Ph.D., highlights their effectiveness:
“Motivational interviewing appears particularly useful in facilitating initial engagement and retention… Cognitive-behavioral approaches appear to be moderately effective and durable in reducing substance use”.
However, therapy isn’t without challenges. Dropout rates in integrated therapy programs can range from 58% to 80%, and patients with severe cognitive impairments may find it difficult to grasp complex coping strategies. Additionally, focusing on one disorder can sometimes exacerbate the other. For instance, exposure therapy for PTSD might heighten anxiety, potentially leading to substance use as a coping mechanism.
Cognitive Behavioral Therapy (CBT)
CBT helps patients identify and manage scenarios that may lead to substance use. Through “functional analysis”, therapists work with patients to pinpoint high-risk situations – such as specific emotions, people, or environments – and develop “skills training” to navigate or avoid these triggers.
For dual diagnosis patients, CBT tackles both conditions simultaneously by reshaping thought patterns and promoting healthier habits like regular exercise and nutritious eating. A meta-analysis of 53 trials found that 58% of participants receiving CBT achieved better outcomes than those in control groups.
CBT also addresses the “Abstinence Violation Effect”, where a single slip often leads to a full relapse. By reducing feelings of shame and hopelessness, CBT helps patients recover from minor setbacks without spiraling back into substance abuse.
For individuals with conditions like schizophrenia, therapists adapt CBT to meet their needs. These modified versions simplify concepts, use concrete language, and incorporate repetition and rewards – such as small monetary incentives for drug-free tests – to ensure accessibility.
Dialectical Behavior Therapy (DBT)
Originally designed for borderline personality disorder, DBT has shown great promise for dual diagnosis patients who experience intense emotional fluctuations that can trigger substance use. This therapy combines acceptance and change, teaching four core skills: mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance.
Distress tolerance skills are particularly valuable for relapse prevention. Patients learn techniques such as deep breathing, self-soothing activities, and strategies to endure emotional crises without resorting to substances. As the Association for Behavioral and Cognitive Therapies explains:
“The stance of a DBT therapist is generally to help the individual learn to ‘replace pills with skills'”.
Research shows that behavioral control – such as eliminating life-threatening behaviors – can often be achieved within four to eight months of comprehensive DBT. Marsha Linehan, the creator of DBT, describes its ultimate goal as helping individuals build:
“a life worth living”.
This focus on creating a meaningful life, rather than just avoiding substances, makes DBT especially effective for those whose substance use stems from emotional pain or emptiness. Full DBT programs include individual therapy, group skills training, phone coaching, and therapist consultation teams. Programs that omit these elements may not achieve the same results.
Motivational Interviewing
Motivational Interviewing is a client-centered approach designed to resolve ambivalence about recovery. It complements CBT and DBT by helping patients explore their personal reasons for change, rather than confronting denial or pressuring them into treatment.
This method guides patients through stages of change, from precontemplation to maintenance. Therapists use OARS – Open questions, Affirmations, Reflections, and Summaries – to help patients uncover their internal motivations.
In a study of cocaine-dependent patients with major depression, those receiving motivational therapy attended more aftercare sessions – seven on average – compared to just two among those in standard care. Improved retention is critical, as therapy can only be effective if patients consistently attend sessions. Motivational Interviewing has demonstrated effect sizes of up to d=0.5.
This approach works best during the early stages of treatment, fostering readiness before transitioning to skill-building therapies like CBT. Starting CBT too early, before a patient feels motivated, can backfire by reducing engagement and creating resistance to treatment. Timing and sequencing these therapies properly is essential for success.
Medication Methods for Preventing Relapse
Medications play a crucial role in stabilizing brain chemistry and alleviating withdrawal symptoms – two major triggers for relapse. Unlike therapy, which develops coping mechanisms over time, medications provide immediate relief by reducing cravings and restoring chemical balance. When combined with therapy, these approaches create a well-rounded strategy to combat relapse in individuals with dual diagnoses.
Timing is critical. Medications work best after a period of abstinence, as ongoing substance use can obscure psychiatric symptoms and lead to incorrect diagnoses.
Dual diagnosis treatment generally focuses on two main approaches. Medication-Assisted Treatment (MAT) addresses substance use disorders by mitigating withdrawal symptoms or blocking the pleasurable effects of drugs. On the other hand, psychiatric medication management targets the mental health conditions that often drive individuals toward substance use.
Depression, for example, is a major risk factor for overdose. Research shows that 23.6% of people who died from an overdose had a depressive disorder diagnosis. This highlights the importance of addressing both mental health and substance use issues simultaneously.
Medication-Assisted Treatment (MAT)
MAT combines FDA-approved medications with counseling and behavioral therapies, offering what the Substance Abuse and Mental Health Services Administration (SAMHSA) refers to as a “whole-patient” approach. These medications not only reduce cravings but also modify the brain’s response to substances, lowering the likelihood of relapse during challenging times.
For opioid use disorder, three medications are commonly used:
- Methadone: A long-acting opioid agonist that eases withdrawal symptoms and cravings by fully activating opioid receptors.
- Buprenorphine: A partial opioid agonist that reduces withdrawal symptoms with a lower risk of misuse or overdose. It was also the first opioid medication that could be prescribed in office settings.
- Naltrexone: An opioid antagonist that blocks opioid receptors entirely, preventing any euphoric effects if a relapse occurs.
For alcohol use disorder, three medications are widely used:
- Acamprosate: Helps restore chemical balance and alleviates long-term withdrawal symptoms.
- Disulfiram: Causes unpleasant physical reactions when alcohol is consumed, discouraging drinking.
- Naltrexone: Reduces alcohol’s rewarding effects, making it less appealing.
Interestingly, around 14% of opioid use disorder treatment episodes also involve co-occurring alcohol use disorder. However, individuals with both conditions are 25% less likely to receive medication treatment compared to those with only one diagnosis.
While MAT focuses on substance use, psychiatric medication management addresses the mental health conditions that often lead to self-medication.
Psychiatric Medication Management
Psychiatric medications are essential for stabilizing mental health conditions that often drive substance use. Untreated issues like depression, anxiety, or psychosis can push individuals toward substances as a form of self-medication.
Antidepressants, particularly Selective Serotonin Reuptake Inhibitors (SSRIs) like sertraline and fluoxetine, are often the first choice for treating comorbid depression. They are favored for their safety and low risk of interactions with alcohol. Older antidepressants, such as tricyclic antidepressants (TCAs) like imipramine, may be more effective in some cases but come with higher risks of side effects and drug interactions. As Dr. Muhammad N. Iqbal explains:
“Antidepressant medication may be successful in alleviating depressive symptoms, and possibly reducing substance use, among individuals with a substance use disorder and depression”.
Antipsychotic medications, particularly second-generation antipsychotics (SGAs) like clozapine, olanzapine, and risperidone, are crucial for individuals with schizophrenia and co-occurring substance use. These medications not only manage psychotic symptoms but may also reduce cravings. Dr. Thomas M. Kelly highlights:
“Clozapine appears to be the most effective of the antipsychotics for reducing alcohol, cocaine and cannabis abuse among patients with schizophrenia”.
Mood stabilizers like lithium and valproate are commonly used to manage bipolar disorder. Valproate, in particular, has shown promise in reducing heavy drinking in individuals with bipolar disorder. For anxiety disorders, buspirone is a safer option for managing generalized anxiety and alcohol dependence, as it avoids the misuse risks associated with benzodiazepines.
ADHD medications present unique challenges in dual diagnosis cases. Approximately 23% of individuals with substance use disorders also have ADHD. Adolescents with depression are more than twice as likely to use illicit drugs compared to their peers without depression. While stimulants are often more effective than non-stimulant options like atomoxetine, they carry a risk of misuse. Extended-release amphetamines, however, have a lower misuse rate (0.5%) compared to immediate-release forms (1.1%).
| Medication Category | Common Examples | Role in Relapse Prevention |
|---|---|---|
| Opioid Use Disorder (MAT) | Methadone, Buprenorphine, Naltrexone | Reduces cravings and withdrawal; blocks opioid effects |
| Alcohol Use Disorder (MAT) | Disulfiram, Acamprosate, Naltrexone | Discourages drinking or reduces alcohol’s appeal |
| Antidepressants | SSRIs (Sertraline, Fluoxetine) | Treats depression and anxiety to prevent self-medication |
| Antipsychotics | Clozapine, Risperidone, Olanzapine | Manages schizophrenia symptoms and reduces cravings |
| Mood Stabilizers | Valproate, Lithium | Stabilizes mood swings in bipolar disorder |
Therapy vs. Medication: Side-by-Side Comparison
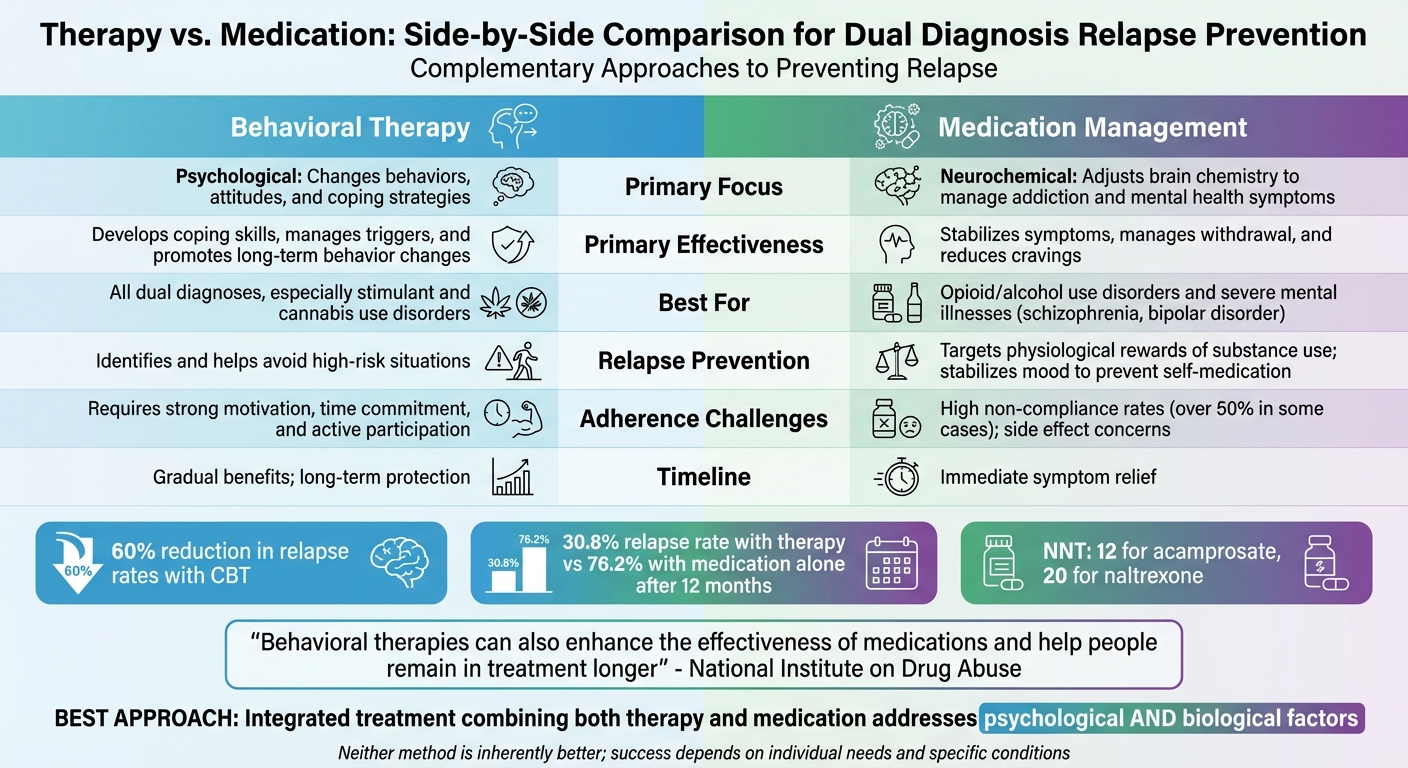
Therapy vs Medication for Dual Diagnosis Relapse Prevention
Therapy and medication take different but complementary paths in preventing relapse for those with dual diagnoses. Medication works on the neurochemical level, adjusting brain chemistry to manage addiction and mental health symptoms. In contrast, therapy addresses the psychological side, helping individuals change behaviors, attitudes, and coping strategies. Neither method is inherently better; their success depends on the specific condition and the person’s unique needs.
The main difference lies in their focus. Medication reduces the physical cravings for substances, while therapy helps individuals handle stressors – like certain people, places, or emotions – that can lead to relapse. As the National Institute on Drug Abuse highlights:
“Behavioral therapies can also enhance the effectiveness of medications and help people remain in treatment longer”.
This difference also means each method comes with its own challenges when it comes to sticking with the treatment.
Adherence is a hurdle for both approaches. For medication, compliance can be tough; over 50% of patients with schizophrenia don’t stick to their prescribed regimens. Issues like side effects and cognitive difficulties often get in the way. On the other hand, therapy requires a lot of effort – patients need to stay motivated, commit their time, and engage deeply with the process.
In relapse prevention for dual diagnoses, the focus may shift depending on the condition. Behavioral therapy is the go-to for stimulant and cannabis use disorders, as there are no FDA-approved medications for these addictions. However, for opioid and alcohol use disorders or severe mental health conditions like schizophrenia and bipolar disorder, medication is often a cornerstone of treatment.
Here’s a quick comparison of the two approaches:
| Feature | Behavioral Therapy | Medication Management |
|---|---|---|
| Primary Effectiveness | Great for developing coping skills, managing triggers, and long-term behavior changes | Effective for stabilizing symptoms, managing withdrawal, and reducing cravings |
| Adherence Challenges | Requires strong motivation, time commitment, and active participation | High rates of non-compliance (over 50% in some cases); concerns about side effects |
| Suitability | Key for all dual diagnoses, especially stimulant and cannabis use | Essential for opioid/alcohol use disorders and severe mental illnesses like schizophrenia and bipolar disorder |
| Relapse Prevention | Helps individuals identify and avoid high-risk situations | Targets the physiological rewards of substance use or stabilizes mood to prevent self-medication |
Pros and Cons of Therapy
When it comes to preventing relapse in individuals with dual diagnoses, therapy has its own set of strengths and limitations. Studies highlight its long-term benefits: for instance, patients who discontinued cognitive therapy had a 30.8% relapse rate over 12 months, compared to a 76.2% relapse rate for those relying solely on medication. As Kathleen M. Carroll, Ph.D., from Yale University School of Medicine, explains:
“Behavioral therapies can play a key role in promoting and maintaining compliance with pharmacologic treatments directed at the psychiatric symptoms, the substance use disorder, or both.”
One of therapy’s greatest strengths is its ability to equip patients with practical coping mechanisms. Cognitive Behavioral Therapy (CBT) helps individuals identify patterns of substance use through functional analysis, while Motivational Interviewing fosters a strong therapist-patient connection that encourages long-term treatment participation. The effectiveness of such approaches is evident in programs like the BTSAS Program, where 59% of participants remained in treatment with clean urine samples, compared to just 25% in the control group. While these benefits are encouraging, therapy is not without its challenges.
Therapy requires active participation, which can be particularly difficult for individuals with severe mental illnesses or those under the influence of substances. Practical barriers, such as cost and logistical issues, further complicate access. In fact, 52% of adults with co-occurring disorders reported receiving no mental health or substance use treatment in the past year.
Another drawback is the time commitment therapy often demands. Unlike medication, which can provide quicker symptom relief, therapy’s benefits tend to unfold gradually during the maintenance phase. Additionally, interventions like Contingency Management may lose their effectiveness once external incentives are removed.
Here’s a quick breakdown of therapy’s pros and cons in this context:
| Advantages | Disadvantages |
|---|---|
| Offers lasting protection after treatment ends (30.8% relapse vs. 76.2% for medication) | Requires active participation, which can be difficult for some |
| Teaches practical coping strategies for triggers | Time-consuming; results take longer to appear |
| Improves medication adherence and retention in treatment | Financial and logistical hurdles limit availability |
| Avoids physical side effects like weight gain or sexual dysfunction | High relapse rates still occur (80–95% for some substances) |
| Encourages reframing lapses as learning opportunities | Positive effects of some methods fade when incentives stop |
While therapy has proven to be a powerful tool for many, its challenges highlight the need for a balanced approach that considers individual needs and circumstances.
Pros and Cons of Medication
Medication brings both benefits and challenges when it comes to preventing relapse in dual diagnosis cases. Antoine B. Douaihy, M.D., from the University of Pittsburgh’s Department of Psychiatry, highlights its potential:
“The use of medications in the treatment of SUD can also play a major role in preventing relapse and facilitating longer periods of abstinence.”
This section dives into the advantages and challenges of using medication for relapse prevention.
One of the biggest strengths of medication is how quickly it can stabilize psychiatric symptoms. For individuals struggling with severe depression, anxiety, or psychosis – conditions that often lead to substance use – this can be life-changing. Medications like naltrexone and acamprosate help curb cravings, while methadone is effective for managing withdrawal symptoms that keep people trapped in substance use cycles. For harm reduction, agonist therapies significantly reduce high-risk behaviors like intravenous drug use, cutting down the chances of contracting HIV or Hepatitis C. To put it into perspective, the Number Needed to Treat (NNT) for acamprosate to prevent a return to drinking is 12, while for oral naltrexone, it’s 20.
However, medications aren’t without their downsides. Side effects can range from mild to severe. For example, disulfiram can cause dangerous reactions, including arrhythmias or even death, if alcohol is consumed. Antipsychotics like clozapine and olanzapine often lead to weight gain and metabolic issues, with clozapine requiring regular blood monitoring. SSRIs, while effective for mood stabilization, frequently cause sexual dysfunction, and older tricyclic antidepressants (TCAs) carry risks like high toxicity and cardiac complications. Methadone, while effective, comes with a high risk of overdose, especially when combined with alcohol or sedatives, and requires strict regulatory oversight.
Adherence is another major hurdle. A study found that only 19% of patients consistently took disulfiram, which means supervised dosing or long-acting injectables may be necessary. Additionally, about 23.6% of accidental overdose deaths involved patients with a depressive disorder, highlighting the difficulty of managing psychiatric medications alongside addiction treatment.
Here’s a side-by-side look at the benefits and challenges:
| Advantages | Disadvantages |
|---|---|
| Quickly stabilizes psychiatric symptoms (e.g., depression, psychosis) | Side effects range from mild nausea to severe reactions |
| Reduces cravings and blocks substance rewards | Low adherence rates (e.g., only 19% consistently took disulfiram) |
| Eases withdrawal symptoms, breaking dependency cycles | Methadone has overdose risks and strict regulations |
| Decreases high-risk behaviors and disease transmission | Antipsychotics may lead to weight gain and metabolic issues |
| Supports long-term therapy engagement | SSRIs often cause sexual dysfunction; TCAs carry cardiac risks |
| NNT: 12 for acamprosate, 20 for oral naltrexone | Limited success with methamphetamine or cannabis disorders |
While medication plays a crucial role in stabilizing symptoms biologically, its success hinges on proper monitoring, adherence, and integration with other treatments. Combining these strategies with therapy can strengthen efforts to prevent relapse in dual diagnosis cases.
Combining Therapy and Medication: The Best Approach for Dual Diagnosis
Preventing relapse in dual diagnosis cases requires more than just therapy or medication alone. Instead, integrated treatment – a coordinated approach combining both therapy and medication – has become the preferred method for managing co-occurring disorders. This strategy consistently delivers better outcomes compared to treatments that tackle each disorder separately or sequentially. By blending the strengths of both methods, integrated care addresses the complex challenges that dual diagnosis patients face.
Medications play a crucial role in stabilizing brain chemistry, while therapy helps patients manage psychological triggers. Together, they create a more effective treatment plan. As Dr. Thomas M. Kelly from the University of Pittsburgh Medical Center explains:
“Creative combinations of psychotherapies, behavioral and pharmacological interventions offer the most effective treatment for comorbidity”.
The evidence backs this up. For example, a study examining the BTSAS program – which integrates Motivational Interviewing, Contingency Management, and medication – found that 59% of participants stayed in treatment and provided clean urine samples, compared to just 25% in a standard care group. Similarly, combining fluoxetine with Cognitive Behavioral Therapy resulted in significant improvements in both alcohol use and depressive symptoms. In cases involving schizophrenia, the use of clozapine helped 54% of patients stop using cannabis and alcohol, while only 8% achieved the same results with risperidone. These findings highlight why combining therapies and medications leads to better outcomes than using either approach in isolation.
Simultaneously treating mental health and addiction is essential. Despite the high prevalence of co-occurring disorders, many individuals fail to receive dual treatment. Addressing only the addiction often leaves psychiatric symptoms unmanaged, which can increase the likelihood of relapse. When substance use stops but mental health issues remain untreated, symptoms can worsen, creating a cycle that leads back to substance use. This interconnected relationship between addiction and mental health demonstrates why integrated care is far more effective than treating each condition separately.
If you’re seeking treatment, look for programs where mental health and addiction specialists work together as a unified team. The Substance Abuse and Mental Health Services Administration (SAMHSA) stresses:
“The best way to serve people with CODs is to offer services and programs that are integrated, comprehensive, person centered, and recovery oriented in their structure, milieu, and practice”.
This collaborative approach ensures that providers communicate consistently, adjust treatment plans as needed, and focus on the whole person rather than isolated symptoms. Such programs embody the comprehensive care necessary for preventing relapse in individuals with dual diagnoses.
Resources from Sober Living Centers for Relapse Prevention
Sober Living Centers provides straightforward guidance on how to prevent relapse in individuals with dual diagnoses. The platform breaks down the three stages of relapse – emotional, mental, and physical – helping people identify warning signs early, before substance use begins again. This approach builds on established dual diagnosis treatments by offering practical advice tailored to each stage of the relapse process.
In addition to educating patients, Sober Living Centers simplifies access to treatment with detailed directories and tools. The site dives into therapy options like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Trauma-Focused Therapy, explaining how these methods can work alongside medication-assisted treatment. The educational materials stress that treating both mental health and substance use disorders together is crucial since addressing only one can increase the risk of relapse.
The platform also provides tools to help users find integrated treatment services, such as dual diagnosis rehab centers, inpatient programs, and sober living homes. These tools include 24/7 confidential support, making it easier for individuals to connect with comprehensive care. Additionally, the site highlights peer support networks like Double Trouble in Recovery (DTR), which are specifically designed for individuals managing both mental health and substance use challenges.
Sober Living Centers also offers practical relapse prevention strategies. These include tips for identifying internal and external triggers, avoiding risky “Seemingly Irrelevant Decisions” (SIDs), and using techniques like urge surfing to manage cravings. The resources emphasize the importance of having a lapse plan and maintaining a balanced lifestyle through activities like exercise and hobbies. By focusing on trigger management and proactive planning, these strategies effectively complement therapy and medication-based treatments.
Conclusion
Preventing relapse in individuals with dual diagnoses requires a combined approach that integrates both medication and therapy. Medications like Naltrexone and Acamprosate help stabilize brain chemistry and reduce cravings, while therapies such as Cognitive Behavioral Therapy (CBT) and Motivational Interviewing address behavioral patterns and equip individuals with essential coping skills. Statistics reveal that nearly 50% of individuals relapse within 12 weeks after inpatient treatment. Yet, among the 9.2 million adults with co-occurring disorders, only 8% receive treatment for both conditions. Integrated treatment – where both disorders are addressed simultaneously within one system – has consistently shown better results in reducing symptoms and preventing relapse compared to sequential or parallel approaches.
The Substance Abuse and Mental Health Services Administration (SAMHSA) underscores this point:
“The best way to serve people with CODs is to offer services and programs that are integrated, comprehensive, person centered, and recovery oriented in their structure, milieu, and practice”.
Treatment plans must be tailored to each individual’s unique circumstances. For example, a person managing depression alongside alcohol use disorder will require a different approach than someone with schizophrenia and cannabis use disorder. Factors like the severity of each condition, the individual’s readiness for change, and their specific triggers all play a role in determining the most effective combination of therapy and medication.
For those seeking guidance, Sober Living Centers offers a wealth of resources. The platform provides information on therapy options, medication-assisted treatments, and directories to locate programs that treat co-occurring disorders. Additionally, it offers educational materials on relapse stages and strategies for managing triggers, helping individuals develop personalized prevention plans.
FAQs
What is the best way to combine therapy and medication for treating dual diagnosis?
The best way to treat dual diagnosis – when someone struggles with both a mental health disorder and a substance use disorder – is through integrated care that tackles both conditions simultaneously. This approach often combines medication tailored to the individual’s needs (like antidepressants, antipsychotics, or medications designed for substance dependence) with therapy, such as cognitive-behavioral therapy (CBT). Together, these methods can help lower the risk of relapse and support better long-term recovery.
CBT stands out because it helps individuals pinpoint triggers, build healthier coping skills, and address the thoughts and behaviors fueling both conditions. By treating mental health and substance use issues together, integrated care creates a path toward greater stability and improved overall well-being. For more information on relapse prevention and recovery tools, check out Sober Living Centers.
How does therapy help prevent relapse in individuals with dual diagnosis?
Therapy plays a crucial role in helping individuals with a dual diagnosis – a combination of a mental health condition and substance use disorder – avoid relapse. It provides practical tools such as coping mechanisms, emotional regulation techniques, and behavioral strategies to navigate triggers and high-risk situations.
Approaches like cognitive-behavioral therapy (CBT) are particularly effective. They focus on identifying and reshaping thought patterns and behaviors that fuel substance use and mental health struggles. Therapy also dives into deeper issues, like trauma or anxiety, which often act as catalysts for relapse. By building self-awareness, resilience, and motivation, therapy not only supports long-term recovery but also helps individuals design relapse prevention plans that fit their specific circumstances.
What makes it difficult to stick to medications in dual diagnosis treatment?
Sticking to prescribed medications can be tough for people dealing with both mental health and substance use disorders, a combination often referred to as dual diagnosis. Several factors can make this difficult, such as unpleasant side effects, a lack of understanding about their condition, or the challenge of managing multiple prescriptions at once. These hurdles can lead to missed doses, which may increase the chances of relapse or worsen symptoms.
Other obstacles include the stigma tied to mental health or addiction, forgetfulness, low motivation, and practical issues like limited access to pharmacies. Tackling these challenges with education, personalized support, and practical strategies can make a big difference in improving medication adherence and reducing the risk of relapse during recovery